Cutting Alcohol May Enhance GLP-1, Obesity and type 2 diabetes are two of the most significant public health challenges of the 21st century. Globally, millions of individuals struggle with excess weight, insulin resistance, and elevated risk for diabetes-related complications. One of the most promising therapies for weight management and metabolic health is the use of GLP-1 receptor agonists (GLP-1 RAs), a class of medications designed to improve glucose control, reduce appetite, and promote weight loss.
However, recent insights from clinical experts suggest that lifestyle factors—particularly alcohol consumption—may significantly influence the effectiveness of GLP-1 therapy. Emerging research indicates that cutting alcohol can enhance GLP-1 outcomes, improve insulin sensitivity, and help patients achieve better metabolic results. In this comprehensive guide, we explore how alcohol impacts GLP-1 therapy, the mechanisms behind these effects, and practical strategies to optimize treatment outcomes.
Understanding GLP-1 and Its Role in Metabolic Health
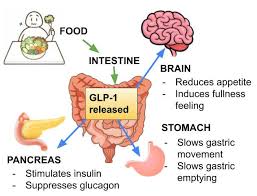
GLP-1, or glucagon-like peptide-1, is a hormone naturally produced in the gut in response to food intake. It plays several critical roles in regulating metabolism:
- Stimulates insulin secretion – GLP-1 promotes glucose-dependent insulin release, helping maintain blood sugar levels.
- Reduces glucagon secretion – Glucagon is a hormone that increases blood sugar. GLP-1 balances its effects.
- Slows gastric emptying – By delaying stomach emptying, GLP-1 helps control appetite and post-meal blood sugar spikes.
- Promotes satiety – GLP-1 reduces hunger signals, assisting with weight loss.
Pharmaceutical formulations of GLP-1, such as semaglutide and liraglutide, are widely prescribed for patients with obesity and prediabetes or type 2 diabetes. Clinical trials consistently show significant improvements in weight loss, glycemic control, and cardiometabolic outcomes with GLP-1 therapy.
How Alcohol Interferes With GLP-1 Function
Alcohol consumption, particularly in excess, has profound effects on metabolic health and hormone regulation. Several mechanisms explain why cutting alcohol may enhance GLP-1 therapy outcomes:
1. Alcohol Impairs Insulin Sensitivity
Alcohol can interfere with the liver’s ability to regulate glucose. Chronic intake may lead to insulin resistance, reducing the effectiveness of GLP-1 in promoting glucose uptake. By reducing alcohol intake, patients may improve insulin sensitivity, allowing GLP-1 to work more efficiently.
2. Alcohol Disrupts Gut Hormone Signaling
GLP-1 is secreted from intestinal L-cells in response to food. Alcohol can damage the gut lining and alter gut microbiota, potentially suppressing GLP-1 secretion. Cutting alcohol restores gut health, optimizing endogenous GLP-1 production and enhancing therapy efficacy.
3. Alcohol Increases Caloric Intake
Alcohol is calorie-dense (7 kcal per gram) and often consumed alongside high-sugar or high-fat foods. Even moderate alcohol consumption can contribute to weight gain, counteracting the appetite-suppressing effects of GLP-1 agonists. Reducing alcohol consumption helps reinforce weight loss achieved through therapy.
4. Alcohol Triggers Inflammation
Chronic alcohol intake promotes systemic inflammation, which is linked to insulin resistance and metabolic dysfunction. By eliminating alcohol, inflammatory markers decrease, creating a healthier environment for GLP-1 to act.
5. Alcohol Affects Brain Signaling
GLP-1 not only acts on the gut but also communicates with the brain to regulate appetite and reward pathways. Alcohol impacts neurotransmitters like dopamine, potentially dampening GLP-1’s effects on satiety and craving reduction. Cutting alcohol restores these pathways, making patients more responsive to therapy.
Clinical Evidence Supporting Alcohol Reduction During GLP-1 Therapy
Several studies and expert opinions support the benefits of reducing alcohol intake when undergoing GLP-1 therapy:
- Improved Weight Loss: Patients who limit alcohol while on GLP-1 medications tend to lose more weight compared to those who continue regular drinking.
- Better Glycemic Control: Alcohol reduction has been shown to lower fasting glucose and HbA1c levels, enhancing GLP-1’s glucose-lowering effects.
- Reduced Side Effects: Alcohol can exacerbate GLP-1-related gastrointestinal side effects, such as nausea or vomiting. Avoiding alcohol reduces these symptoms, improving adherence.
Experts in endocrinology emphasize that lifestyle modifications remain a critical complement to GLP-1 therapy, and alcohol reduction is a particularly impactful strategy.
Practical Strategies for Cutting Alcohol During GLP-1 Therapy
For patients with obesity or diabetes risk, reducing alcohol intake can optimize treatment outcomes. Here are practical strategies:
1. Set Clear Goals
Define how much and how often you plan to drink. Some patients may benefit from complete abstinence, while others may adopt a moderate approach.
2. Replace Alcohol With Healthy Alternatives
Water, herbal tea, sparkling water, or non-alcoholic beverages can satisfy the habit without impacting metabolism.
3. Address Social Triggers
Many drinking habits are social. Plan alternatives for social situations and communicate your health goals to friends and family.
4. Track Progress
Keeping a journal of alcohol consumption, GLP-1 injections, and weight/glucose readings helps reinforce positive changes.
5. Seek Professional Support
Healthcare providers can guide patients in reducing alcohol safely and provide counseling resources if needed.
Additional Lifestyle Interventions to Enhance GLP-1 Outcomes
Beyond alcohol reduction, other lifestyle interventions can amplify GLP-1 therapy:
- Balanced Diet: Focus on high-fiber, low-sugar foods to support satiety and blood sugar control.
- Regular Exercise: Physical activity enhances insulin sensitivity and promotes weight loss.
- Sleep Optimization: Adequate sleep improves appetite regulation and hormone balance.
- Stress Management: Chronic stress can increase cravings and impair glucose control.
Integrating these habits creates a synergistic effect with GLP-1 medications, improving both metabolic and cardiovascular outcomes.
Key Takeaways From Experts
- GLP-1 therapy is highly effective, but its results are significantly influenced by lifestyle factors.
- Cutting alcohol enhances insulin sensitivity, reduces inflammation, and improves weight management, directly supporting GLP-1 outcomes.
- Personalized interventions, including dietary counseling and behavioral support, can maximize the benefits of therapy.
- Patient education is critical: Understanding the interaction between alcohol and GLP-1 empowers patients to make informed choices.
Dr. Jane Matthews, an endocrinology expert, notes:
“Patients who reduce alcohol while on GLP-1 therapy often see faster and more sustainable improvements in weight and glucose control. It’s a simple change with a big impact.”
Conclusion
For patients with obesity and diabetes risk, cutting alcohol may be one of the most powerful ways to enhance GLP-1 therapy outcomes. Alcohol reduction improves insulin sensitivity, reduces inflammation, supports weight loss, and strengthens gut and brain signaling—all of which make GLP-1 medications more effective.
Combined with diet, exercise, and other lifestyle changes, this approach offers a holistic strategy to improve metabolic health, lower diabetes risk, and achieve sustainable weight management.
As research continues to explore the interplay between lifestyle factors and GLP-1 therapy, one thing is clear: small, intentional changes like cutting alcohol can have a profound impact on long-term health outcomes.